Advance Care Planning - My Wishes, ReSPECT Plan, Anticipatory Medications
Anticipatory Medications
Anticipatory prescribing or ‘just in case’ medicines is a key component of high-quality end-of-life care. It ensures that patients can receive prompt relief from distressing symptoms at any time, particularly when oral medications are no longer effective or appropriate.
Advance care planning should routinely include anticipatory prescribing to avoid unnecessary delays in symptom management. Having the appropriate medicines and administration charts readily available in the patient’s home enables timely care and supports a more comfortable and dignified end-of-life experience.
An audit of PCN prescribing identified a variety of medicines, doses, strengths and frequency were being prescribed. This highlighted a need for recommendations and guidance for generalist prescribers, who may only prescribe anticipatory medicines infrequently.
Generalist and specialist palliative clinicians have collaborated to create an EMIS prescribing protocol and supporting documents, which are designed to improve symptom control for patients who are at End-of-Life, to enable more timely administration, more equitable access and to reduce prescribing and administration errors.
The anticipatory medicine protocol is for use by PCNs and OOH providers in Herefordshire and Worcestershire, or anyone who is prescribing anticipatory medicines for patients in their own home or a community residential setting.
The prescription and prescription chart are generated digitally through EMIS Web, or the protocol can be imported into a compatible system. The protocol at the point of use with the patient, is a paper process and copies of documents are left in the patient’s home.
Anticipatory Medicine Protocol
2 Elements
- EMIS
web or imported prescribing protocol – generates digital prescription
& prescription chart to be printed or emailed
- Supporting
guidance and administration documents - ALL to
be printed as a pack and left in patient’s home
- Prescriber
and Administrator Guidance for Subcutaneous Anticipatory Medications PRN &
Syringe Pump
- Administration
Record for Subcutaneous PRN Medicines
- Administration
Record for Syringe Pump Medicines
- Syringe
Pump Observation Chart
- Record
of Medicine Stock
EMIS
web or imported prescribing protocol – generates digital prescription
& prescription chart to be printed or emailed
- Prescriber and Administrator Guidance for Subcutaneous Anticipatory Medications PRN & Syringe Pump
- Administration Record for Subcutaneous PRN Medicines
- Administration Record for Syringe Pump Medicines
- Syringe Pump Observation Chart
- Record of Medicine Stock
The prescribed medicines may include a dose range.
Appropriate training needs to be completed through your training provider.
Seek guidance from a prescriber & never administer outside of your competence.
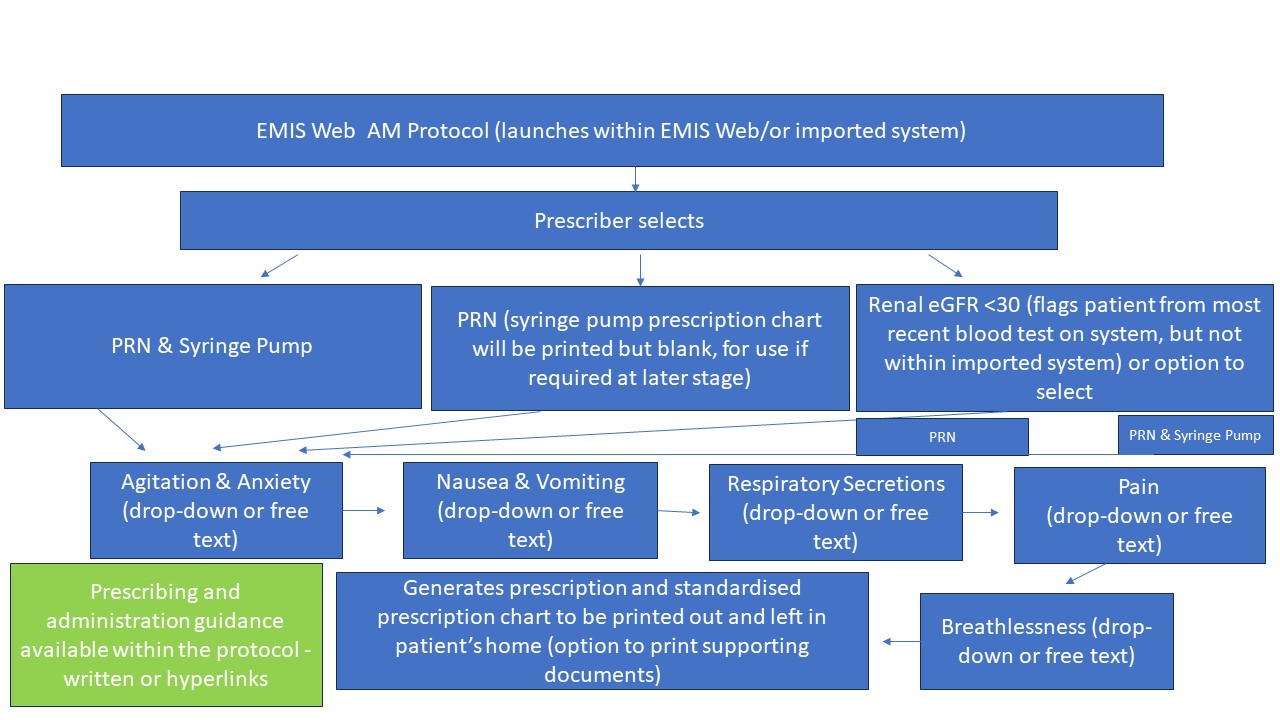
Supporting Guidance & Administration Documents – Version 1.0 in use – ALL NEED TO BE PAPER COPIES IN PATIENT’S HOME
- A
completed chart is generated through EMIS Web protocol (or systems with
protocol imported) - printed at source or emailed to administrator for use in
patient’s home.
- Prescription
chart has 2 sections. Section
1 – As
required drugs & Section 2 – continuous subcutaneous infusion via
syringe pump. Both should always be
available to allow prescribing directly onto the chart in the patient's
home.
- It
is the only prescription chart to be used in the community for anticipatory
medicines.
- Outside
of EMIS web or systems that have not imported the protocol, it can be used as
an editable pdf or printed as a blank chart to be handwritten.
- Guidance
contains information available to EMIS web or imported protocol users around
medicines recommendations, links to guidance, pharmacy stockists and Specialist
Palliative Care (SPC) contacts details.
- Guidance
should be available in patient’s home to inform administrators &
prescribers who do not have EMIS Web protocol access.
- Guidance
contains information available to EMIS web or imported protocol users around
medicines recommendations, links to guidance, pharmacy stockists and Specialist
Palliative Care (SPC) contacts details.
- Guidance
should be available in patient’s home to inform administrators &
prescribers who do not have EMIS Web protocol access.
- A
new page 5a should be commenced every 24 hours from midnight.
- Additional
pages for the same 24 hours require page numbering – 5 b,c etc.
- Requested
by administrators to allow calculating total dose of medicines easier &
reduce administration errors through miscalculation.
4. Administration Record for Syringe Pump Medicines (page 6)
5. Syringe Pump Observation Chart (page 7)
6. Record of Medicine Stock (page 8)
Organisation & Administrators Responsibilities
- Each organisation will provide training and education to registered clinicians who administer anticipatory medicines through established education processes
- Guidance includes prescribing medicine dose ranges for improved timely symptom control
- Registered clinicians who administer should not administer outside of their competence or if they have not received education or training around assessment for dose range
- Support and advice should always be obtained and documented
- Any updates on version will be agreed as a working group and organisations advised to update to current version
- Individual organisations will be responsible to update systems & clinicians.
Patient Information
Patient Information
 |
 |
 |
|---|